EXPLORUS SURGICAL
Minimize Dissection with Autograft Iliac Crest Tricortical Graft Harvesting Device
Experience advanced bone harvesting with minimal soft tissue disruption and enhanced surgical efficiency.
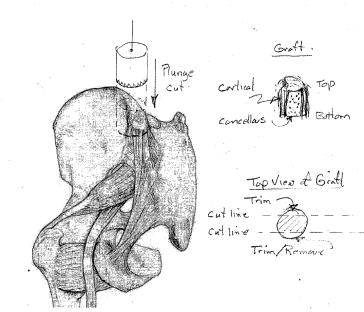
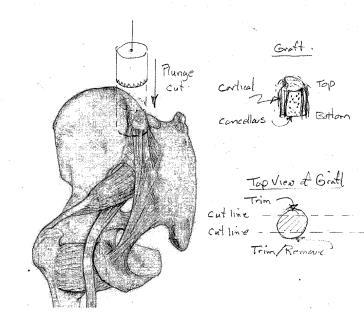
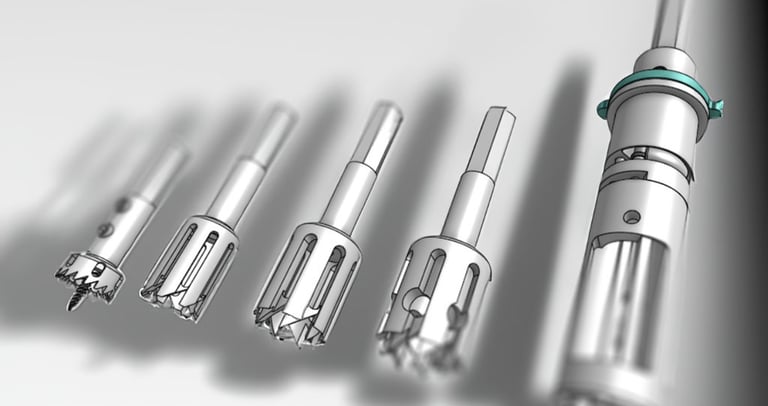
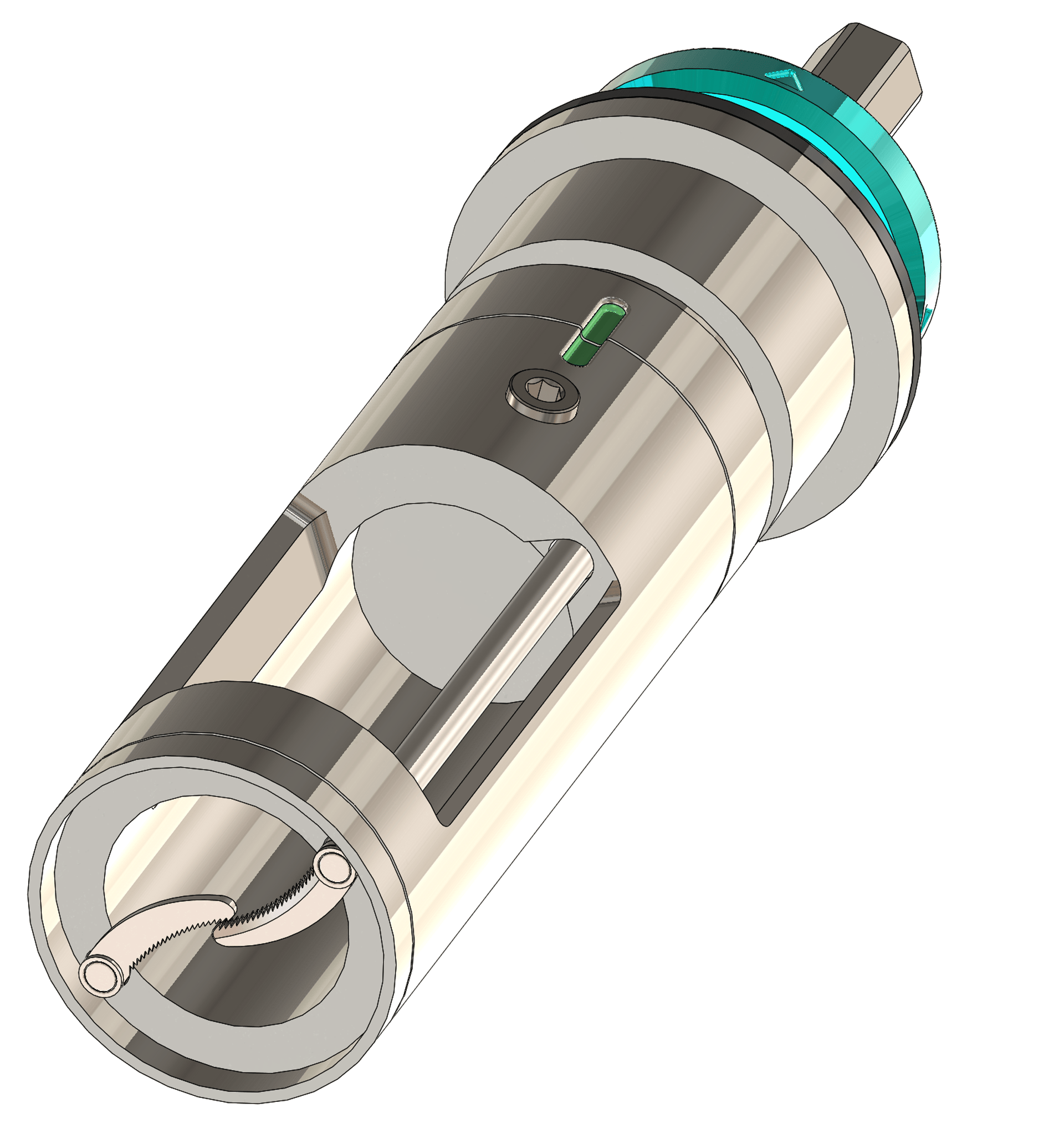
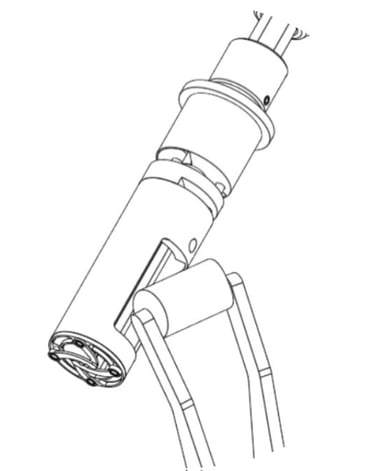
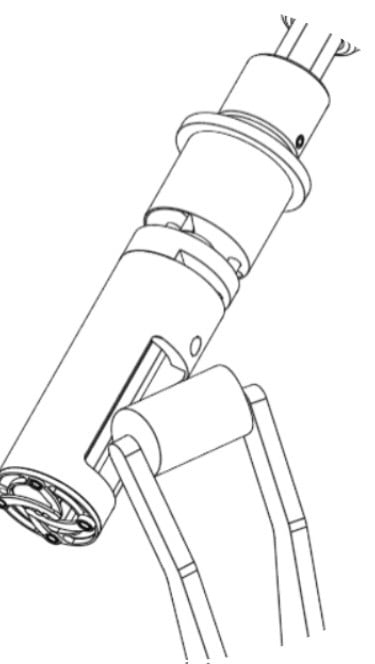
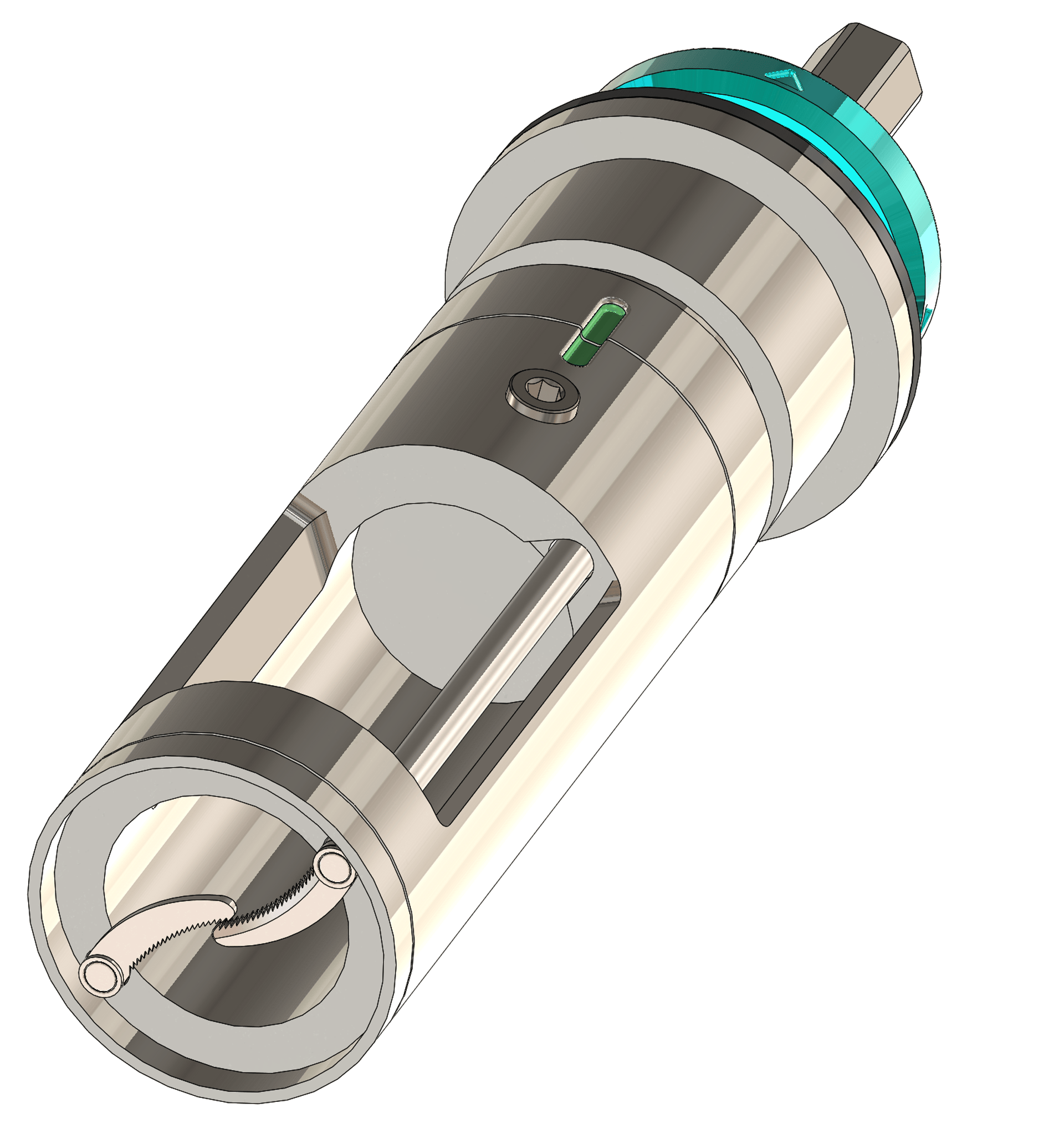
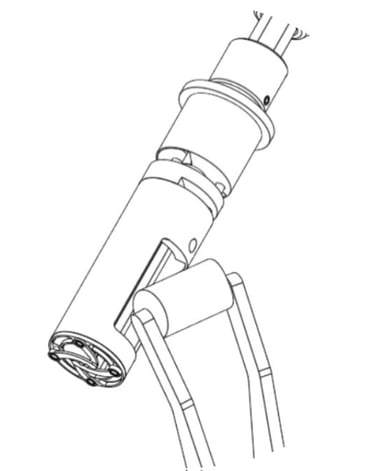
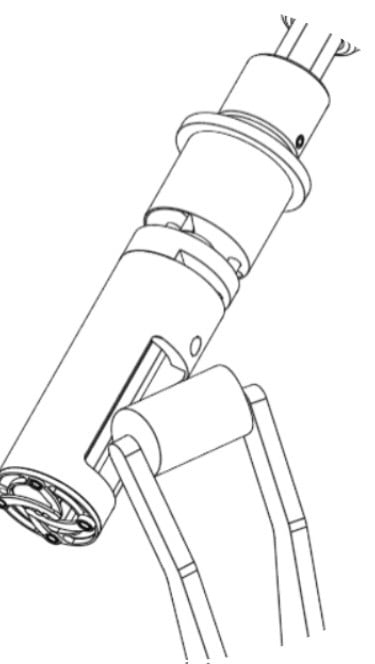
This is not an ordinary bone harvesting trephine. This is a new technology large 12mm to 20mm diameter bone harvesting trephines armed with built-in curettes at the push of a button to address the base of the bone core to detach and harvest cancellous bone cores; harvesting the cortico-cancellous bicortical graft and tricortical graft. This is the trephinated curettage technique.
Takes a bone out!
One single harvest provides sufficient bone volume for 1-level ACDF spinal fusion.
Harvests the tricortical graft within 3 minutes. The 'trephine' component performs the downward plunge-cut to create a bone core, followed by the curettes to 'curettage' to rapidly procure it.




Research and Development at Barrow Neurological Institute, USA
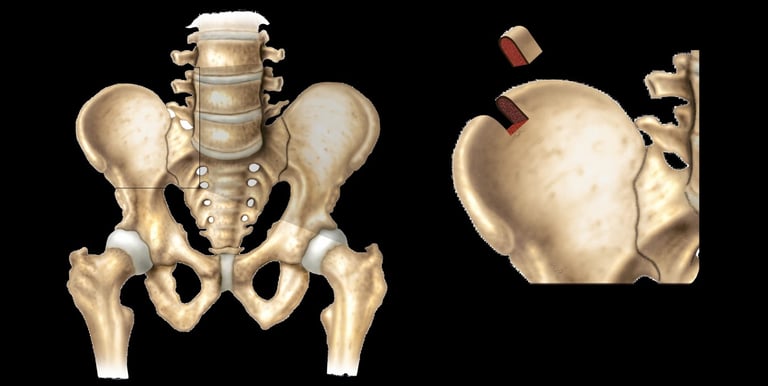
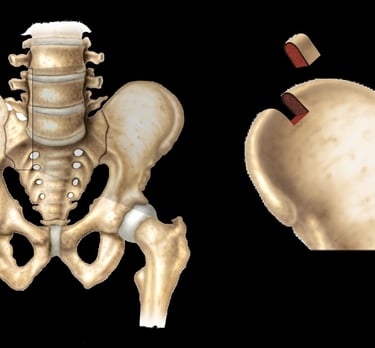
TRICORTICAL GRAFT


Because of the razor sharp teeth, the down plunge-cutting takes 30 seconds, as the total bone cutting time is done is 60 seconds, the tricortical graft is securely procured.
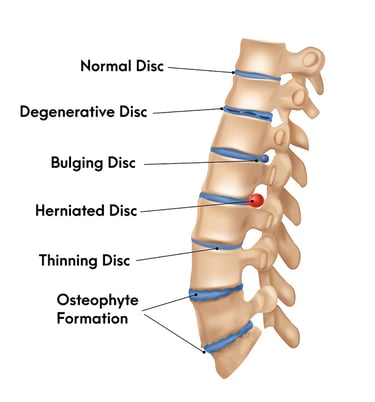
INTRODUCTION
Worldwide, there are millions of patients each year suffering from bone-related illness due to trauma, degenerative diseases, infections or oncology that require orthopaedic intervention involving bone grafts. Bone autografts remain the gold standard since there are no issues with histocompatibility or disease transmission while possessing the ideal characteristics: osteogenicity, osteoconductivity and osteoinductivity.
Autogenous bone grafting is a powerful surgical tool because it can offer the surgeon ample cortical or cancellous bone to achieve osseous union. Despite promising advances in the field of bone regeneration, the use of autologous bone grafts remains the “gold standard” of therapy. Although enormous efforts have been made in bone regeneration therapy, autologous bone grafting is still a necessary and frequently used procedure.
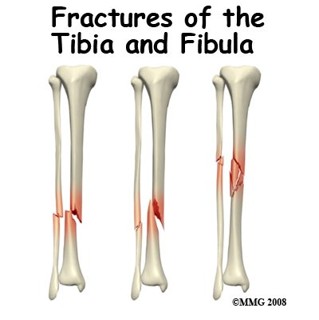
Bone grafting procedures span several specialties and are especially used in orthopaedic, trauma, and reconstructive surgery. The most common indications for grafting are employed in defects resulting from fractures, non-union, tumours, and arthrodesis, followed by osteomyelitis and maxillofacial operations. Iliac Crest Bone Graft (ICBG) has long been considered the gold standard harvesting site. Within the iliac crest, the anterior portion is the most used harvest site. Bone grafting is common, and complications are often underestimated. Nevertheless, donor site morbidity after the harvesting of bone grafts from the anterior iliac crest remains a problem. Despite this, the use of autologous bone grafts remains the “gold standard” treatment for bone loss due to trauma, inflammation, and old age; for the reconstruction of bone structures after tumour excision; and for the filling of cyst defects.
Traditional reliance on the gold standard of ICBG has been tempered by associated morbidity and complications, fostering the quest for alternatives. However, despite the advances in synthetic bone substitute material production, autologous iliac crest bone graft (ICBG) continues to be the gold standard because it meets all the expected needs. Most synthetic bone graft substitutes lack appropriate osteoinduction, osteoconduction, and osteogenesis. In addition, ICBG does not carry the risk of disease transmission, does not cause immunogenic reactions, and inherits excellent regenerative and remodelling capabilities. Less invasive options to harvest iliac bone can reduce morbidity, and trephine harvest is a simple technique with low morbidity and perioperative and long-term pain. Autograft Iliac Crest Bone Graft (ICBG) harvest using a trephine by a minimally invasive approach offers significant advantages.
The anterior iliac crest is the most common donor site for autologous bone grafting. Techniques for anterior iliac crest bone grafting include the curettage technique, bicortical or tricortical technique, trapdoor technique, and trephine technique. It is recommended to pay attention to the complications of anterior iliac crest grafting, namely pain, nerve injury, hematoma formation, infection, incisional hernia, vascular injury, and donor site fracture; the incidence of complications is 20.6%, most of which are persistent pain at the donor site, incision hematoma, infection.
Trephine ICBG harvest minimizes soft tissue dissection, periosteal elevation, and cortical disruption. Using this trephine technique of ICBG harvest by a minimally invasive approach eliminates perioperative complications, and reduces pain in both perioperative and long-term assessments. Compared to historical outcomes, trephine harvest provides sufficient graft with comparable or improved results relative to other minimally invasive approaches, and significantly improves outcomes and patients’ satisfactions relative to traditional open techniques.

Innovative Bone Harvesting Solutions
At Explorus Surgical, we specialize in advanced enlarged 12mm to 20mm diameter trephine ICBG harvesting system devices with increased capacities that can harvest ample cancellous and cortical bone to achieve osseous union and reduce soft tissue dissection with enhanced surgical precision for optimal patient outcomes.


150+
15
Trusted by Surgeons
Proven Results
Bone Harvesting Solutions
Minimize soft tissue dissection and enhance recovery with our advanced trephine ICBG harvest device.

Advanced Harvesting Device
Our trephine ICBG device minimizes disruption while ensuring effective bone harvesting for optimal results.
Efficient Bone Collection
Experience reduced periosteal elevation and cortical disruption with our innovative bone harvesting technology.

This New Technology for the 'Trephinated Curettage Technique' was jointly researched and developed by Barrow Neurological Institute and St. Joseph’s Hospital and Medical Center, Phoenix, AZ 85013, USA
Traditional Bone Harvesting Techniques
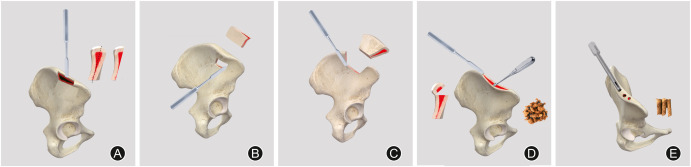
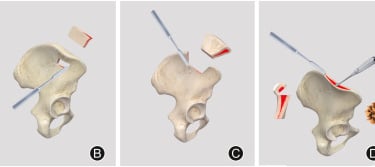
(A) Unicortical, (B) bicortical, (C) tricortical, (D) curettage, and (E) trephination techniques.
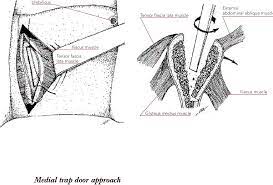
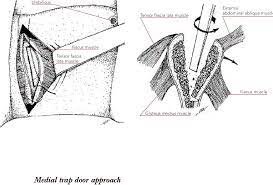
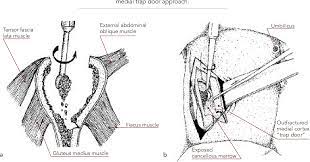
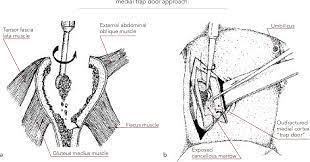
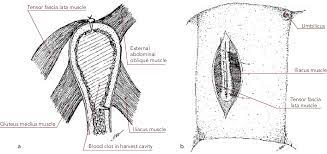
Traditional Trapdoor Method
The anterior iliac crest is the most common donor site for autologous bone grafting. Traditional techniques for anterior iliac crest bone grafting include the conventional curettage technique, bicortical or tricortical technique, trapdoor technique, and trephine technique. It is recommended to pay attention to the complications of anterior iliac crest grafting, namely pain, nerve injury, hematoma formation, infection, incisional hernia, vascular injury, and donor site fracture; the incidence of complications is 20.6%, most of which are persistent pain at the donor site, incision hematoma, infection.



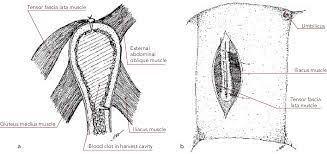
TREPHINE TECHNIQUE
Trephine ICBG harvest minimizes soft tissue dissection, periosteal elevation, and cortical disruption. Using this trephine technique of ICBG harvest by a minimally invasive approach eliminates perioperative complications, and reduces pain in both perioperative and long-term assessments. Compared to historical outcomes, trephine harvest provides sufficient graft with comparable or improved results relative to other minimally invasive approaches, and significantly improves outcomes and patients’ satisfactions relative to traditional open techniques.
Trapdoor methods involve any procedure where a bone flap (or 'trapdoor') is made in the iliac crest from which subcortical bone graft is removed before the flap is replaced to restore the cortical anatomy. This method is 'open', as the cortex is intentionally split to access cancellous bone.
The trapdoor method is used to longitudinally split the medial and lateral edges of the iliac crest, expose the cancellous bone between the medial and lateral plates, preserve the inner plate, and a gouge harvests the cancellous bone of the iliac crest. It has been suggested that trapdoor methods are associated with a greater admission time and analgesia requirement compared with closed methods (e.g. trephination) for ICBG.
TREPHINATED CURETTAGE TECHNIQUE
The purpose of this trephinated curettage technique aims to optimize and to standardize harvest techniques, ample bone graft volume, postoperative pain, functional limitations, and complications of ICBG. In this way, ICBG can be harvested as corticocancellous or cancellous bone graft, depending on the structural integrity desired. The most common complications associated with ICBG harvest are donor site pain and cosmetic deformity due to the iliac crest defect. Major complications include deep infection, fracture, and neurovascular injury. Surgeons must be familiar with relevant anatomy, harvest techniques, bone graft volume, and potential complications associated with iliac crest bone graft to decrease morbidity.
Considering the clinical advantages based on the previous literature, the trephination curettage technique can be recommended for autograft ICBG harvesting. On the other hand, meticulous handling should be followed to minimize the complications, particularly the penetration of the ilium. Since the trephination technique is performed in a blinded fashion, the three-dimensional structure of the ilium should be kept in mind. Another issue to be considered to prevent iliac bone perforation is the adjustment of the depth of the trephine. It was reported that the penetration risk is higher in cases where the trephination depth is more than 30mm, and therefore the depth of the trephination should be controlled, and to stay within a 30mm pelvis depth limit.
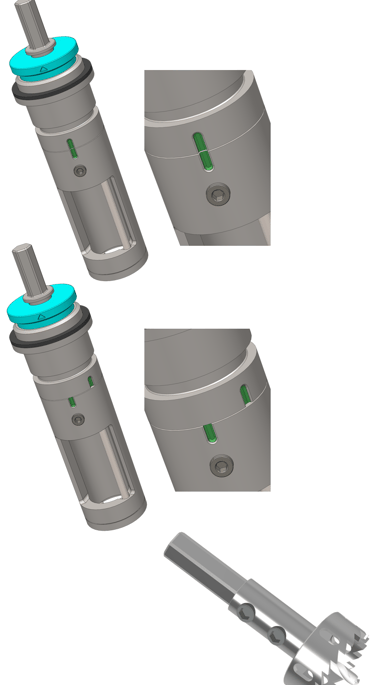
Simply allow the instrument to do its own work, no forced efforts required, use a high speed, consistent light pressure; at the end of the down plunge-cut, then simply press and activate the button and the curette will automatically and completely detach the bone core within 20 seconds, clean and even, and ready for procurement. Instructions, workshop demonstrations, and training are available.
PHILOSOPHY
Currently the “gold standard” for bone grafting is an autograft. If an autograft isn't a good option for the patient, the next best option is normally an allograft. Allograft bone is harvested from cadaveric tissue donors and has been used for many years due to its osteoconductive and osteoinductive properties. However, allograft incorporation into the host bone is slower and less complete compared to autograft. There is also a risk of disease transmission and immune rejection. The main underlying reason for slower and less complete allograft incorporation into native bone is particularly related to lack of vascularisation. The affinity and bone conduction ability of allogeneic bone cells are weak, and osteoblasts have difficulty adhering to and differentiating on their surfaces.
Unfortunately, most synthetic bone graft substitutes lack appropriate osteoinduction, osteoconduction, and osteogenicity. Some show potential, like rhBMP-2 Bone Morphogenetic Protein-2 but were also associated with potential serious complications including ectopic bone formation and possible cancer risks. The fusion rates with alternative bone graft substitutes like BMP-2 is still unclear and fusion rates range widely between studies. Several studies investigated the complication spectrum of BMP-2, including carcinogenicity, and reported a wide range of potential complications, complication rates, and controversial conclusions.
CAGES
To avoid associated problems of graft harvesting, intervertebral cages are an alternative, but cannot provide biological fusion. The major issue with Ti alloys is its low bone-bonding ability; thus, increased research has been done on surface chemical and physical and morphology modifications to improve bone bonding. PEEK polyether ether ketone (PEEK) fusion cage provides stability similar to that of Ti alloys, and in some cases improves durability, strength and overall biomechanical profile. PEEK has radiographic properties that allow surgeons to better monitor possible migration and the success of the implant. However, the primary issue with PEEK is that it is hydrophobic and unable to sufficiently bond to bone to achieve solid fusion, the PEEK cage has few hydrophilic groups, high biological inertia and a smooth surface, and can easily be wrapped by fibrous tissue which cannot provide conditions for the adhesion of osteoblasts, resulting in weak osseointegration ability. This may be associated with cage migration and pseudarthrosis (non-union).
Traditionally, the trephination technique is a well-known bone marrow biopsy method that has been used for diagnostic purposes. Later, the same technique was modified and described as a bone graft harvesting method by enlarging the trephine diameter, and has been used for many years. The trephination technique is a “Closed Method” and has become popular because it can be performed in a smaller incision, and fewer complications have been reported compared to the conventional curettage technique. However, the adequate volume of obtained graft is important for most orthopedic procedures, especially if the size of the bone defect is large. The autograft tricortical iliac crest graft has a wide range of indications.
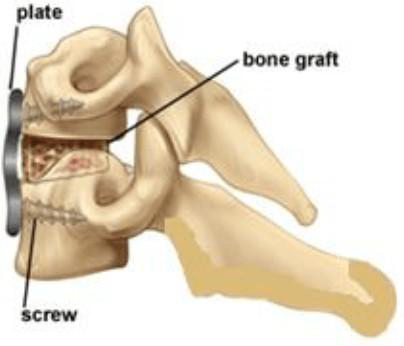
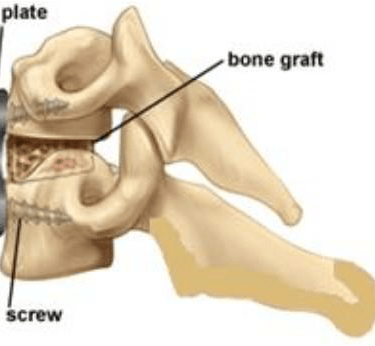
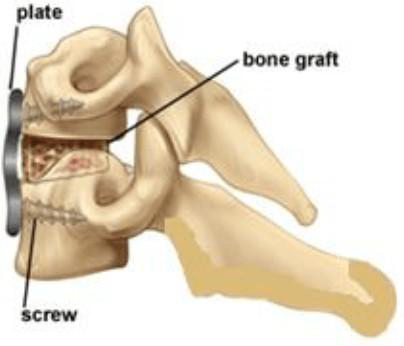
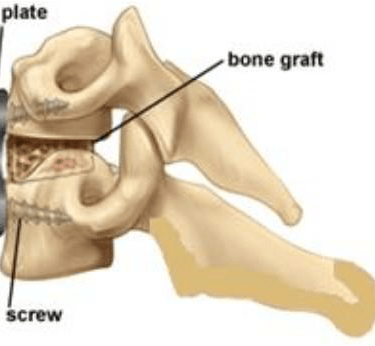
Autograft tricortical iliac crest graft was most often chosen as the gold standard for choice of graft material for ACDF by surgeons. ACDF surgery with stand-alone tricortical iliac crest autograft also has good fusion rates and satisfactory neurological recovery. Although fusion rates may be higher with instrumented fusion, with plating within 1 year of surgery, standalone grafts can produce good results while reducing the cost of implants. Thus, this is still a viable option for surgeons to consider.
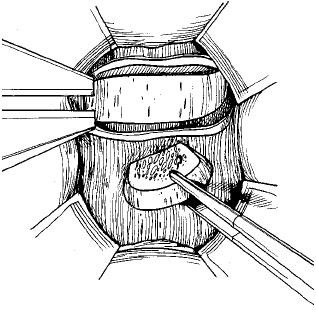
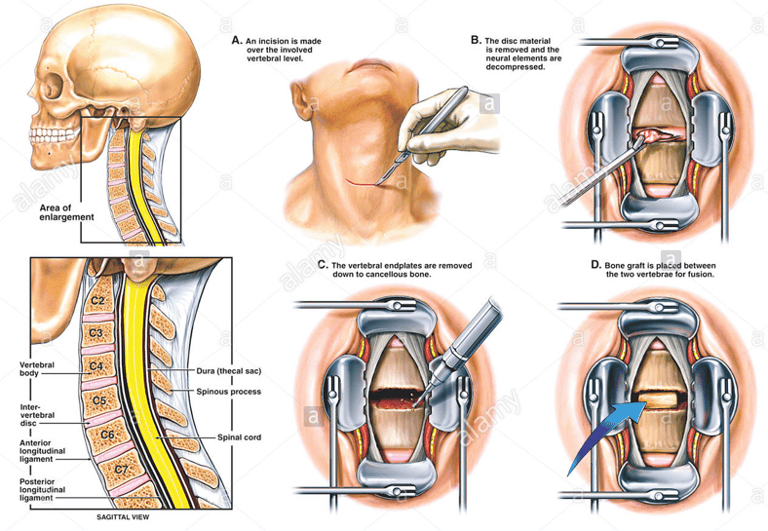
ACDF, or Anterior Cervical Discectomy and Fusion, is a surgical procedure performed on the cervical (neck) spine to relieve pressure on the spinal cord and nerve roots caused by a damaged or herniated disc. The procedure involves removing the problematic disc and then fusing the adjacent vertebrae together using a autograft iliac crest tricortical bone graft to stabilize the spine.
Placement of a Standalone Smith Robinson Tricortical Graft into a prepared spine disc space.
If you ever imagined that this could be possible:


tricortical graft HARVESTER DEVICE
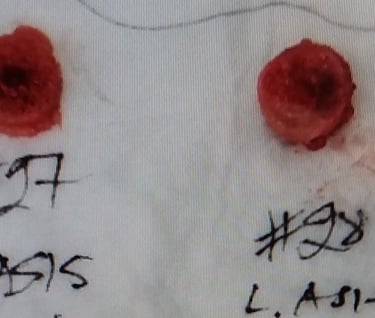
tricortical graft
tricortical graft
If you ever imagined that this could be possible:


tricortical graft HARVESTER DEVICE
tricortical graft
tricortical graft
Surgeons Feedback
Discover how our device transforms bone harvesting with minimal disruption.
“The device is useful and successful for harvesting bone grafts. It has some important advantages, such as ensuring a more quick harvest when compared to the traditional method.
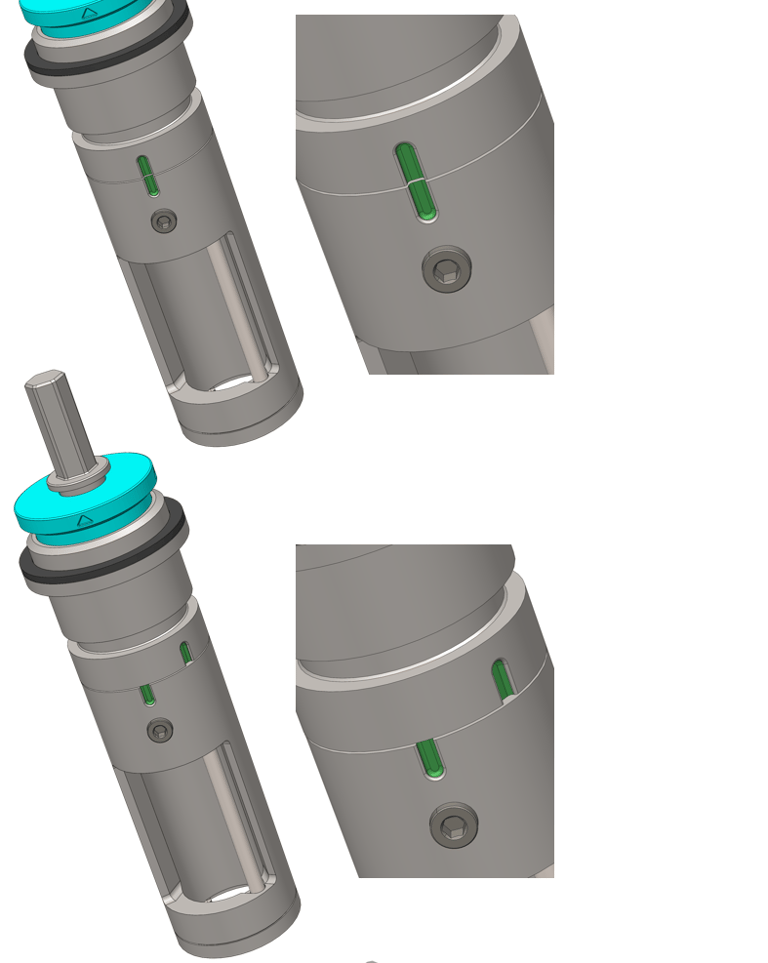
The color-coded indicator green-line sign at the deployment moment allows you to know exactly when the curettage is completed and allows for a bone graft harvest within a smaller incision using a smaller retractor, most likely resulting in less bleeding and postoperative pain.
The bone core comes out in a perfect cylindrical shape that can be directly used as bone graft for ACDF anterior cervical spine discectomy and fusion.
The iliac bone is an ideal site for use of this device and the bone seems to be in good shape when it is used in a cervical fusions.
The availability of different sizes of this devices could allow bone graft harvests for different procedures such as posterior facet distraction and fusion, and anterior and posterior lumbar fusions.”
Dr. Brian P. Kelly Ph.D.
Dr. Anna G.U.S Newcomb M.S.
Dr. Jennifer Lehrman M.S.
Dr. Bernardo de Andrada-Pereira M.D.
Efficiency
Minimizing dissection for optimal autograft ICBG bone harvesting. This is a patented and FDA registered and listed medical device product.
Innovation
+852 9079-9080
© 2025. All rights reserved.
Explorus Surgical
Mr. Ricky Au M.Sc.
Biomedical Engineer
Dr. Brian P. Kelly Ph.D.
Email: brian.kelly@commonspirit.org
Dignity Health
St. Joseph’s Hospital and Medical Center
Barrow Neurological Institute
350 West Thomas Road, Phoenix,
AZ 85013. USA